SOAP Notes. Whether you’re a new grad or seasoned clinician, perfecting your treatment note is a crucial part of any speech therapist’s practice.
Speech therapy SOAP notes document important data and paint a picture of how the client participated in a session. That’s not always easy. A speech-language pathologist’s (also known as “SLP”) schedule is often filled with back-to-back clients throughout the day.
Having a clear understanding of what SLP SOAP notes are, and how to write one both thoroughly and efficiently can be a huge help to SLPs. This helps them feel confident that they documented the necessary information for insurance and legal purposes while not falling behind on paperwork or getting backed up on time.
SLP SOAP notes are a written document that reports on what was done in a therapy session. It should be written the same day as the session occurred. This timely documentation ensures accurate and up-to-date documentation is completed. Additionally, SLP SOAP notes must be completed the same day as the service because they are attached to charges for the session.
The SOAP note can be written after the session. Or, if the SLP uses an easily accessible, concise SOAP note template, the note can be written during the last few minutes of the session itself. TheraPlatform offers a built-in SLP SOAP note template that is clear, consistent, and concise. This allows SLPs to complete the soap note template during the session, making documentation with back-to-back therapy sessions a breeze.
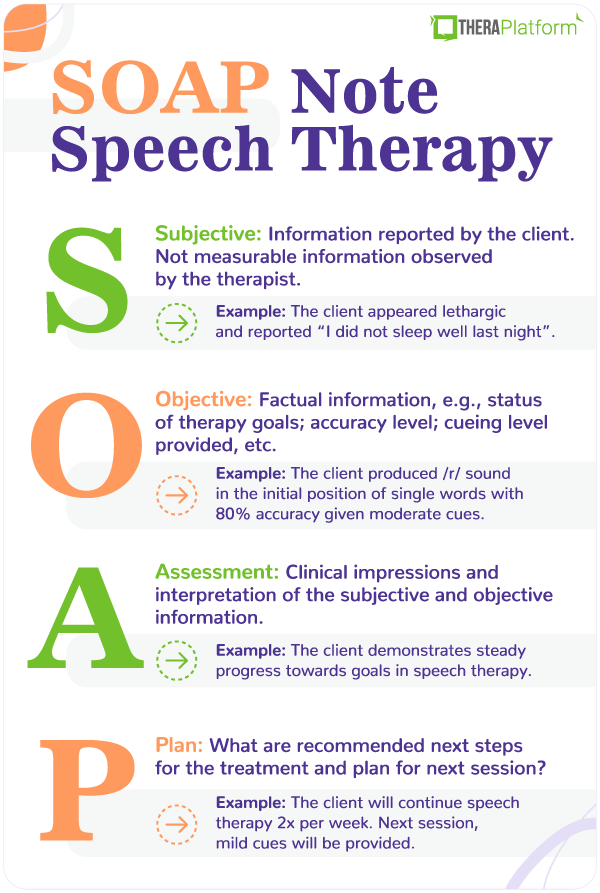
SOAP stands for the 4 sections that make up the therapy note: Subjective, Objective, Assessment and Plan.
It may be shared with the client and/or his or her caregiver, as well as insurance companies. Here’s a closer look at what makes up a SOAP note, and the do’s and don’ts to keep in mind when writing each section along with a SOAP note example.
This is a brief statement that describes a client’s state from the therapist’s point of view.
The information in this section isn’t measurable, and can be gathered both from the therapist’s observations and any information given by the caregiver who accompanies the client to the session.
1. Johnny appeared alert, and transitioned into the therapy room without difficulty. He was engaged and participated in all therapeutic activities that were presented.
2. Alice became upset and clung to her mother upon entering the therapy room. She frequently put her head down and refused to participate in tasks.
3. Cayden appeared lethargic and his mother reported, “he didn’t sleep well last night”. He was engaged and interactive when provided with positive reinforcement and praise.
The objective section is all about stating the facts. The information an SLP writes here must be measurable or quantitative. This usually includes reporting on therapy goals and stating the data that the client achieved for each goal targeted during the session.
When thinking of this section, think percentages, numbers, accuracy level, and scores.
Here, the speech-language pathologist will also state whether each therapy goal was targeted, not targeted, met, not met, or progressing.
1. Johnny produced the /r/ sound in the initial position of single words with 80% accuracy given moderate cues. (Goal Met for 2 out of 3 consecutive sessions)
2. Olivia identified common objects in 7 out of 10 opportunities given minimal cues. (Goal Progressing/Not Met)
3. Allison used irregular past tense verbs at the sentence level with 50% accuracy independently. (Goal progressing/not met)
In the Assessment section of a SOAP note, a speech-language pathologist analyzes and interprets the information documented within the first two sections (the Subjective and Objective sections).
1. Ethan continues to demonstrate steady progress towards goals in speech therapy.
2. Logan’s behavior is impeding his progress towards goals in speech therapy.
3. Mila’s production of the /th/ sound improved by 15% compared to her previous session.
In this final section of the SOAP note, the therapist writes the recommended next steps for the client’s treatment.
State any recommended changes for the next therapy session. For example, “The next therapy session will focus on recording Alex’s speech and encouraging him to monitor it for articulation errors”.
One part of writing a SOAP note is knowing what information to include. The other part is knowing how to document this information. Remember, clear, consistent, and concise are words an SLP should keep in mind when writing a SOAP note.
You want to write it in a way that readers can easily understand the information. Some clinical terminology will be used. However, the note should describe the client’s performance during a session in a way that others who may not have a clinical background can still understand.
Let’s take a look at a clear SLP SOAP note example vs. a SOAP note example that is less clear.
Objective: Client produced the /r/ sound in the initial position of single words with 80% accuracy given moderate cues. (Goal met for 2 out of 3 consecutive sessions)
Objective: Client was able to accurately produce /r/ while reading a story about rabbits. He had more difficulty producing the final /r/ than the medial /r/, and was stimulable for corrections with verbal and tactile cueing. Client was excited that he will have a baseball game today. He liked the book but started crying during the game.
In the second, less clear SOAP note example, the longer description of the client’s performance is unclear to the reader. The specific goal targeted is not easy to determine. The reader is unsure of what word position the goal is for the /r/ sound to be produced.
The objective section in the less clear SOAP note example also leaves the reader questioning at what level the sound is being targeted (ex: single words or sentences). The second SOAP note example also includes extraneous information that is not clinically relevant. Professionally worded statements about the client’s state (ex: engaged, uncooperative) should be included in the “Subjective” part of the SOAP note.
The first, clear SOAP note example on the other hand, would be easier for the audience to understand. Only the most important clinical information is included. The objective section here clearly states the target sound, word position, level of hierarchy, and percentage that provides an objective report on the client’s performance.
Another reason speech pathologists should keep their SLP SOAP notes clear? To fulfill the purpose of the note. The purpose of SLP SOAP notes is to clearly and accurately document a client’s diagnosis, the treatment being provided, and his or her progress.
SLP SOAP notes should appear consistent over time. If a client is seen for ongoing therapy at a given frequency (ex: weekly or monthly), the format of the SLP SOAP notes should look standardized. The specific clinical information such as the therapy goals, client’s state, and progress, will of course differ from one session to the next.
Using a SOAP note template makes it easy for an SLP’s SOAP notes to appear consistent overall. For one thing, it is simple for the SLP to input information about the session into a SOAP note template. Secondly, when using a SOAP note template, others can track and compare documentation over time. This can be important for the reader (such as an insurance reviewer) to easily compare documentation over a span of time to see if the client is demonstrating overall progress by receiving speech therapy.
Consistency with SOAP note templates means information is documented in the same place and format from one session to the next.
SLP SOAP notes should be concise.
SLP SOAP notes should contain approximately 1 small paragraph per section. Some sections may have more information than others.
For example, the SLP may only need to check boxes of statements on a SOAP note template that provide statements such as, “Recommend continue therapy per plan of care”, or “Client continues to demonstrate improvements in Speech Therapy.”
The entire note itself should not exceed 1 to 2 pages. Remember, to serve its purpose to provide parents, other professionals, and insurance reviewers necessary clinical information, the note should be succinct.
Using an SLP SOAP note template makes writing notes fast, efficient, and comprehensive. Here’s a complete SLP SOAP note example:
S: Johnny appeared alert, and transitioned into the therapy room without difficulty. He was engaged and participated in all therapeutic activities that were presented.
O: Client produced the /r/ sound in the initial position of single words with 80% accuracy given moderate cues. (Goal Met for 2 out of 3 consecutive sessions.) Client used personal pronouns accurately in 6/10 opportunities given minimal cues (Progressing/Goal not met.)
A: Johnny continues to demonstrate steady progress towards goals in speech therapy.
P: It is recommended Johnny continue with the current treatment plan of 2 times per week for 30 minutes per session, for an estimated duration of 180 days.
Electronic medical record (EMR) and practice management software, such as TheraPlatform, can help make note taking fast, flexible and accurate.
Having an EMR with built-in note templates, such as SOAP, can help speech-language pathologists stay organized and write more consistent and concise speech therapy notes each time.
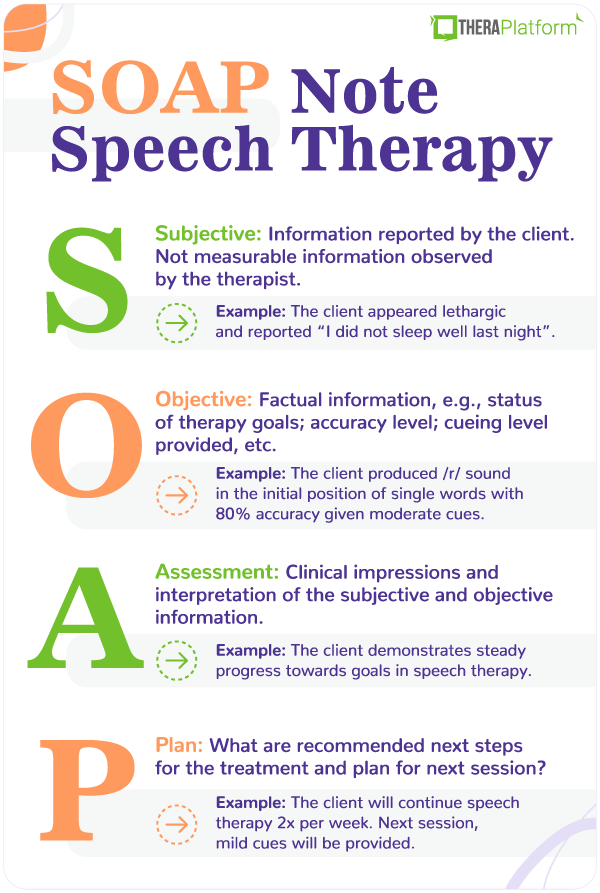
TheraPlatform’s built-in therapy note template library screenshot
Search TheraPlatform’s built-in note therapy note template library based on your profession and edit templates to meet your needs.
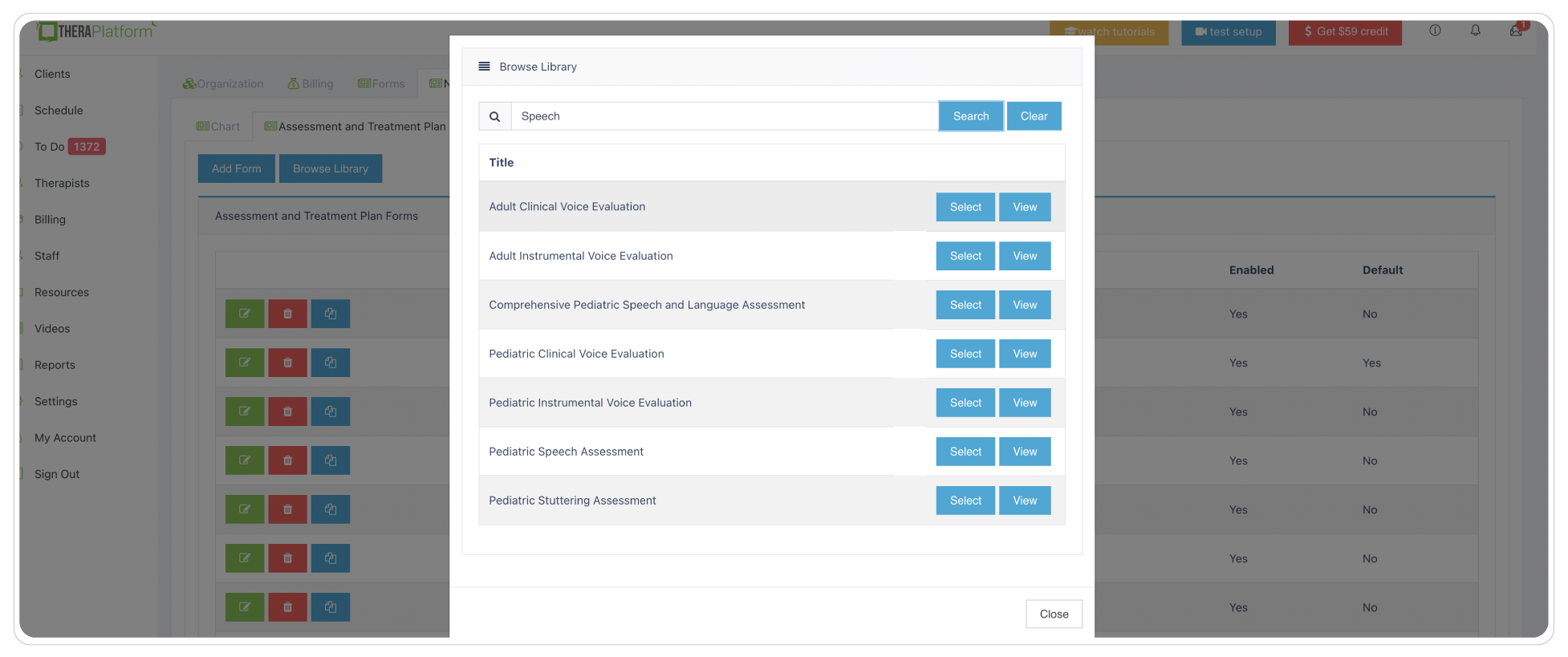
Different SLPs have their own ways of documenting speech therapy sessions. Some love SOAP note templates to help organize subjective, objective, assessment and plan information. Other SLPs prefer just one field that allows them to type their narrative. While other SLPs incorporate checkboxes on their note templates for repetitive information such as techniques used or mental status. Having a robust and easy-to-use note template builder is the key to having such flexibility.
Screenshot of TheraPlatform’s form builder
Leverage existing templates or make them your own with new fields like checkboxes, buttons or pick lists.
Whether you are a covered entity or not under HIPAA, creating and storing your speech therapy notes in a secure, encrypted system to prevent breaches will ensure your client’s data is safe and give you peace of mind. TheraPlatform follows bank-level security standards and provides private practices with a signed BAA.
Start 30-day Free Trial and explore TheraPlatform. HIPAA Compliant Video and Practice Management Software for Therapists.
You may have clients on your caseload who request speech therapy notes for their own records, or superbill clients who need them in case of insurance audit. Having a secure way to share your notes is no brainer.
TheraPlatform’s EMR for speech therapists, allows SLPs to share speech therapy notes with clients via client portal in a HIPAA-compliant and secure way.
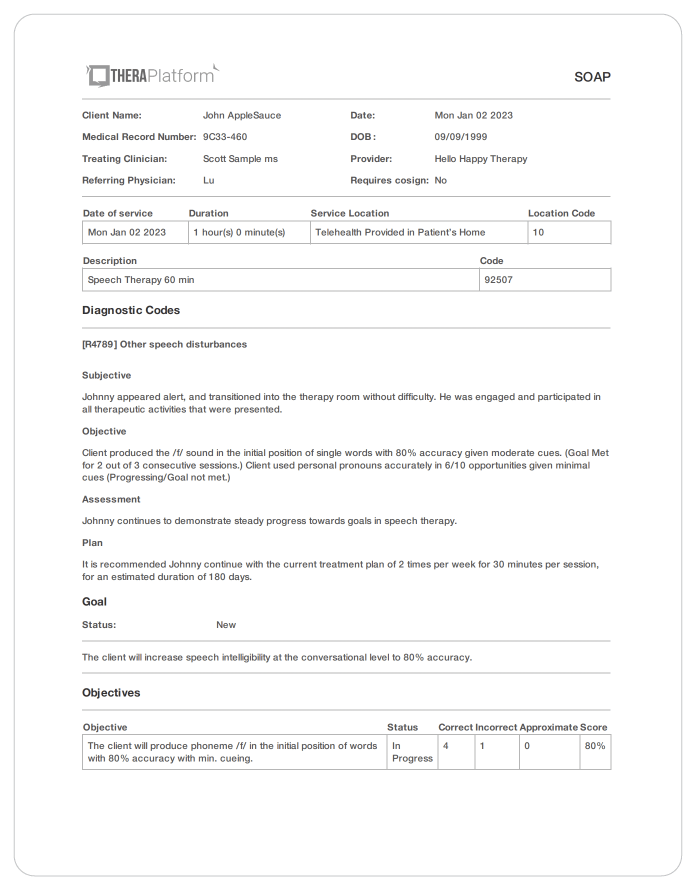
Speech therapy SOAP note created with TheraPlatform. Therapists can share notes with clients with a couple of clicks of a button.
TheraPlatform's Pro and Pro Plus plans offer documentation features with the ability to request signatures from clients on notes. Your client can also download and print this document.
Some information that SLPs type on SOAP notes might repeat from session to session and a copy note feature on TheraPlatform, allows clinicians to copy notes from previous sessions. They can still edit the copied note and add more information to it too.
Having efax integrated into an EMR such as TheraPlatfrom eliminates maneuvering between two services, saves time and lowers cost as incoming and outgoing documents like SOAP notes, and other documents are sent via efax.
Remember, clear, consistent, and concise are words speech therapists should keep in mind when writing an SLP SOAP note. SOAP note templates like those offered on TheraPlatform can make writing SLP SOAP notes much easier. In addition, TheraPlatform has a number of features to make practice management more efficient including scheduling, billing and claims. TheraPlatform, an all-in-one EHR, practice management and teletherapy tool was built for therapists to help them save time on admin tasks. They also offer a 30-day free trial. No credit card required.